Periodontal Disease Treatment
Periodontal Disease Treatment
Published Date
Last Updated
- What is Periodontal Disease? | The “Silent Disease” Affecting 80% of Japanese People
- Do You Have These Symptoms? | Periodontal Disease Self-Check
- Causes of Periodontal Disease | Review Your Lifestyle to Reduce Risks
- Periodontal Disease Treatment Flow
- Common Questions About Periodontal Disease (FAQ)
- View Other Treatments
What is Periodontal Disease? | The “Silent Disease” Affecting 80% of Japanese People
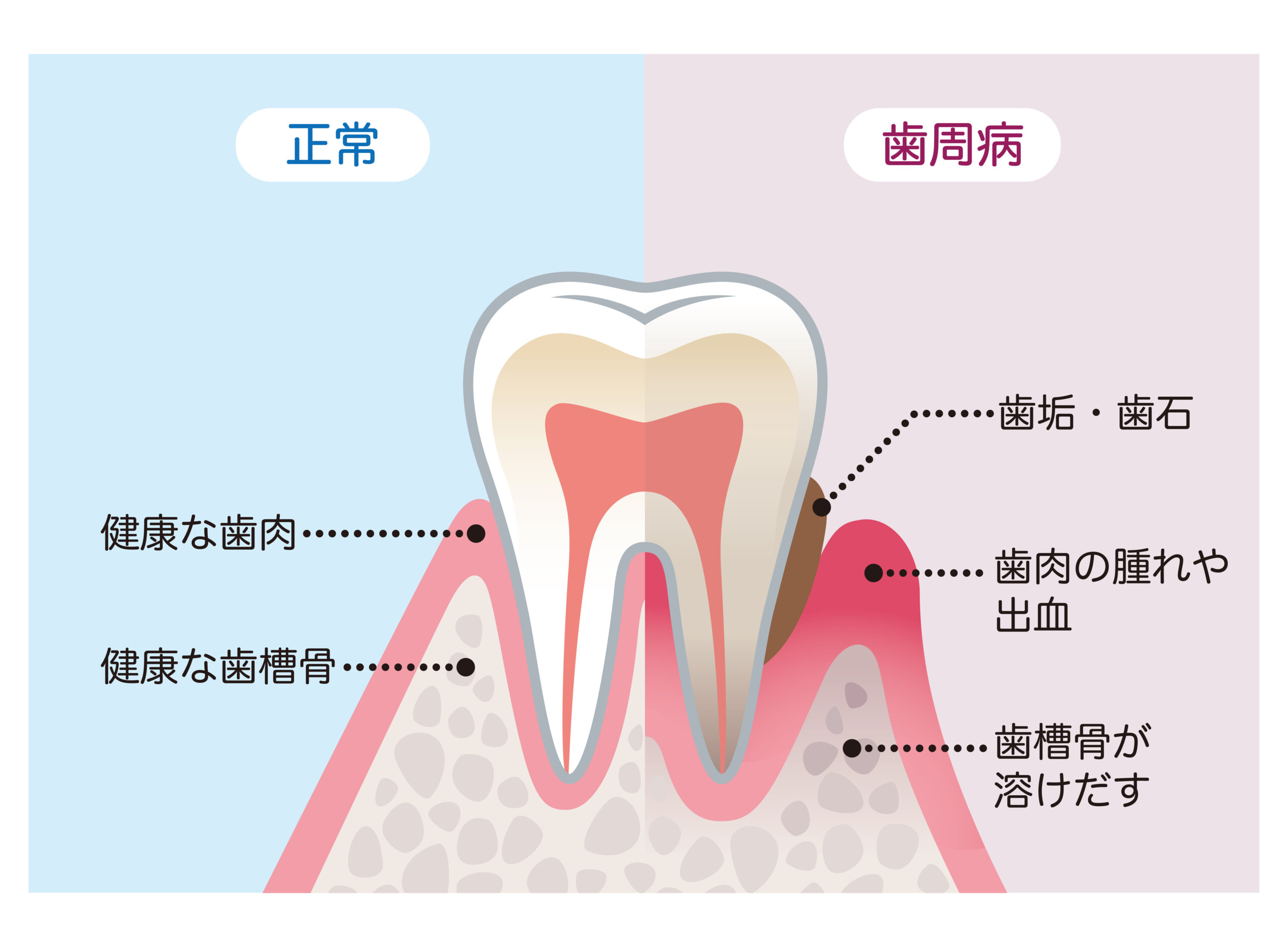
Periodontal disease is a condition where inflammation occurs in the tissues surrounding and supporting the teeth (gums, periodontal ligament, alveolar bone, etc.). Since there are often no noticeable symptoms in the early stages, it is also called the “silent disease.” It can progress unnoticed, and in severe cases, may lead to tooth loss. According to surveys by the Ministry of Health, Labour and Welfare, about 80% of Japanese adults suffer from periodontal disease, making it truly a national affliction.
Periodontal disease progresses through the following stages:
- Gingivitis: Inflammation occurs in the gums, causing them to become red, swollen, and prone to bleeding. At this stage, improvement is possible with proper brushing and professional cleaning at a dental clinic.
- Mild Periodontitis: Inflammation spreads beyond the gums to the bone supporting the teeth (alveolar bone). Grooves called “periodontal pockets” form between the teeth and gums, making it easier for plaque and calculus (tartar) to accumulate.
- Moderate Periodontitis: Periodontal pockets deepen further, and destruction of the alveolar bone progresses. Teeth may become loose, and pus may discharge from the gums.
- Severe Periodontitis: A significant portion of the alveolar bone is destroyed, and teeth become very loose. Eventually, teeth may fall out.
It is known that periodontal disease negatively impacts not only oral health but also overall systemic health. Links have been pointed out with conditions such as diabetes, heart disease, stroke, and preterm/low-weight births.
Periodontal disease, known as the “silent disease,” shows almost no symptoms in its early stages. Therefore, early detection and treatment through regular dental check-ups are extremely important.
Do You Have These Symptoms? | Periodontal Disease Self-Check
If even one of the following applies to you, you may have periodontal disease. Please visit a dental clinic soon.
- Gums bleed when brushing
- Gums are red and swollen
- Gums feel itchy or irritated
- Teeth feel loose
- Gaps have started appearing between teeth
- Teeth look longer (gums have receded)
- Concerned about bad breath
- Mouth feels sticky upon waking up in the morning
- Difficulty chewing hard foods
- Sensitivity to cold
Periodontal Disease Self-Check
If even one applies, you might have periodontal disease. We recommend visiting a dental clinic soon.
Causes of Periodontal Disease | Review Your Lifestyle to Reduce Risks

The main cause of periodontal disease is plaque that accumulates between teeth and gums. Plaque is a mass of bacteria, and the toxins released by these bacteria cause inflammation in the gums, leading to the progression of periodontal disease.
If plaque control (removal of plaque) is insufficient, plaque hardens into calculus (tartar). The rough surface of calculus makes it easier for more plaque to adhere, exacerbating periodontal disease.
Additionally, the following factors increase the risk of periodontal disease:
Oral Environment Factors
- Calculus (Tartar): Calculus is calcified plaque strongly adhering to the tooth surface. Its rough surface facilitates further plaque attachment, worsening periodontal disease.
- Malocclusion (Misaligned Teeth): Poor teeth alignment makes brushing difficult, leading to easier plaque accumulation.
- Interproximal Caries (Cavities Between Teeth): Cavities between teeth are hard to reach with a brush and prone to plaque buildup, increasing periodontal risk.
- Ill-fitting Restorations: Fillings or crowns that do not fit properly create gaps where plaque can easily accumulate, causing periodontal disease.
- Mouth Breathing: Mouth breathing dries the mouth, reducing saliva’s self-cleaning action and increasing periodontal risk.
Morphological Factors of Teeth, Mucosa, etc.
- Tooth Shape: Certain tooth shapes can create areas difficult to reach with a brush, allowing plaque to accumulate.
- Gingival Abnormalities: Abnormal gum shapes can make plaque accumulation easier or brushing more difficult.
- Abnormal Frenulum Position: An abnormal position of the frenulum (the fold inside the lip or cheek) can hinder brushing and allow plaque buildup.
Food and Drink Factors
- Food Texture: Soft or sticky foods adhere easily to teeth, contributing to plaque.
- Thermal Stimuli from Food/Drinks: Excessively hot or cold items can irritate the gums and worsen inflammation.
Deterioration of the Oral Environment
- Pocket Deepening: As periodontal disease progresses, pockets deepen, making plaque and calculus accumulation easier.
- Gingival Recession: Receding gums expose tooth roots, increasing the risk of sensitivity and root cavities.
- Gingival Enlargement: Swollen gums make plaque accumulation easier.
Lack of Awareness and Practice of Plaque Control
- Not knowing or practicing correct brushing methods
- Not using supplementary cleaning tools like interdental brushes or dental floss
- Not attending regular dental check-ups
Influence of Bite (Occlusion)
- Occlusal Trauma: Excessive force on specific teeth damages periodontal tissues, worsening the disease.
- Bruxism (Teeth Grinding): Grinding applies excessive force to teeth and periodontal tissues, potentially worsening periodontal disease.
- Premature Contact: When some teeth contact earlier than others, it places excessive load on those specific teeth, worsening periodontal disease.
- Oral Habits: Habits like cheek leaning or tongue thrusting that place stress on teeth and periodontal tissues increase risk.
Systemic Factors
- Infectious Diseases: Infections can lower immunity, making periodontal disease more likely to worsen.
- Metabolic Diseases: Conditions like diabetes are risk factors for worsening periodontal disease.
- Endocrine Disorders: Hormonal imbalances increase periodontal disease risk.
- Allergic Diseases: Allergic reactions can make gums prone to inflammation.
- Blood Disorders: Increase the risk of gum bleeding and infection.
- Nutritional Deficiencies: Poor nutrition lowers the resistance of periodontal tissues, worsening the disease.
- Age: Risk increases with age.
- Gender: Women may have increased risk due to hormonal changes (pregnancy, menopause).
- Stress: Can lower immunity and potentially worsen periodontal disease.
- Fatigue: Can lower immunity and potentially worsen periodontal disease.
- Smoking: The biggest risk factor for periodontal disease.
- Medications: Some drugs (e.g., Phenytoin, Nifedipine, Cyclosporine) have side effects that worsen periodontal disease.
There are various causes beyond those listed above. Let’s start by understanding the condition of your own mouth through a regular check-up.
Periodontal Disease Treatment Flow

At our clinic, periodontal disease treatment follows this general flow:
1. Consultation, Examination, Diagnosis
First, we carefully listen to your oral condition, concerns about periodontal disease, wishes, etc. Then, we perform the following examinations to accurately diagnose the stage of periodontal disease progression.
- Basic Periodontal Examination:
- Intraoral Examination: We examine the entire mouth, checking the condition of teeth, gums, bite, etc.
- Periodontal Tissue Examination: Using an instrument called a probe, we measure the depth of periodontal pockets and check for gum inflammation, bleeding, and tooth mobility. For “periodontal disease examination,” we comprehensively judge these results to diagnose the stage.
- Plaque Adhesion Check: We show photos and other materials to analyze areas where brushing is difficult. Depending on the situation, we may use disclosing solution to confirm plaque adhesion and provide guidance on appropriate brushing methods.
- X-ray Examination: X-rays are taken to check the condition of the supporting bone (alveolar bone), root morphology, etc.
- Intraoral Photography: Photos of the inside of the mouth are taken to record the condition before and after treatment. This allows patients to visually confirm their own oral condition.
Based on these examination results, we formulate a treatment plan tailored to each patient and explain it clearly.
2. Scaling (Calculus Removal)
Scaling is the removal of calculus (tartar) and plaque attached to the tooth surface using a specialized instrument called an ultrasonic scaler. Since calculus harbors periodontal bacteria, removing it via scaling is fundamental to periodontal treatment.
When using the ultrasonic scaler, we take care to minimize pain and sensitivity, especially for those with sensitive teeth. If you usually experience sensitivity to cold, please don’t hesitate to inform us. We will adjust the instrument’s intensity or use hand scalers depending on your condition.
3. Periodontal Tissue Examination (2nd Time)
After initial treatments like scaling, following a certain period (usually one week or more), we conduct another periodontal tissue examination to check if gum inflammation and pocket depth have improved. The results determine the subsequent treatment plan.
4. Scaling and Root Planing (SRP)
If the second periodontal tissue examination reveals calculus attached deep within the gums or deep pockets (5mm or more), a procedure called Scaling and Root Planing (SRP) is performed. SRP is the removal of calculus, plaque, and contaminated cementum from the unseen root surfaces below the gumline using specialized instruments. “Periodontal root planing” is a crucial step in improving periodontal disease.
SRP is often performed under local anesthesia, so there is usually minimal pain. Our clinic also employs various techniques to reduce patient burden, such as using fine instruments and combining with ultrasonic scalers. Depending on the severity, SRP may be performed over several sessions.
Generally, if pockets are 5mm or deeper, instruments may not fully reach the bottom, lowering the success rate of calculus removal. Tooth morphology, such as concavities or grooves, can also reduce removal efficiency. After assessing tooth morphology through examination, we remove calculus as thoroughly as possible. Because it requires delicate handling and monitoring of gum improvement, scaling and root planing often takes about 4 to 6 sessions. The “periodontal treatment duration” varies depending on severity and method, but please understand that SRP requires a relatively longer treatment period.
5. Periodontal Tissue Examination (3rd Time)
After SRP, following a certain period (usually 4 to 6 weeks), we conduct another periodontal tissue examination to check if the periodontal condition has improved. The results determine the subsequent treatment plan.
6. Periodontal Surgery (If Necessary)
Periodontal surgery is a surgical treatment performed when periodontal disease has progressed and improvement cannot be expected with basic treatments like SRP. SACHI Dental Clinic proposes appropriate periodontal surgery based on the patient’s oral condition.
Main types of periodontal surgery include:
- Periodontal Pocket Curettage: Surgery to remove infected tissue within the periodontal pocket.
- Flap Surgery: Surgery involving incising the gum to expose the root surface for thorough removal of calculus, plaque, and infected tissue.
- Periodontal Tissue Regeneration Therapy: Treatment using special materials (like Emdogain) to promote the regeneration of periodontal tissues (alveolar bone, periodontal ligament, etc.) lost due to disease.
Our clinic proposes the optimal periodontal surgery based on the patient’s oral condition and wishes.
In some cases, if more specialized treatment is deemed necessary, we may refer you to advanced medical institutions like university hospitals.
7. Regular Check-ups & Maintenance
After periodontal treatment is completed, or when symptoms stabilize, the patient transitions to Regular Check-ups & Preventive Dentistry.
Common Questions About Periodontal Disease (FAQ)

- Can periodontal disease be cured?
- Periodontal disease can be improved with appropriate early treatment. However, periodontal tissue once lost cannot be completely restored to its original state. Therefore, it is important to halt the progression of the disease through treatment and maintain a healthy condition. Also, since periodontal disease is prone to recurrence, regular maintenance after treatment is necessary.
- Is periodontal treatment painful?
- Periodontal treatment, such as calculus removal and cleaning inside periodontal pockets, may involve some discomfort. Our clinic strives to minimize pain by using methods like topical anesthesia and electric anesthesia injectors.
- How long does periodontal treatment take?
- The duration of periodontal treatment varies depending on the severity of symptoms and the treatment method. Mild cases might improve with a few visits, but severe cases can take several months to over a year. We formulate a treatment plan based on each patient’s condition and explain it carefully.
- How much does periodontal treatment cost?
- Basic periodontal treatment is generally covered by health insurance. However, some treatments like periodontal tissue regeneration therapy are not covered. We will explain the details during counseling. If you want to know about “periodontal treatment costs” beforehand, please inquire by phone.
- How can I prevent periodontal disease?
- Daily brushing is the most important factor in preventing periodontal disease. Use not only a toothbrush but also supplementary cleaning tools like interdental brushes and dental floss to thoroughly remove plaque between teeth and in periodontal pockets. Regular check-ups at a dental clinic for professional care like calculus removal and PMTC are also crucial. For “periodontal disease prevention,” both self-care and professional care are essential.
- Is there anything else I can do besides brushing?
- Besides brushing, paying attention to the following can help prevent periodontal disease:
- Maintain a balanced diet
- Refrain from smoking
- Manage stress
- Get sufficient sleep
- Receive appropriate treatment for systemic diseases like diabetes
View Other Treatments
Treatment Menu
Types of Ceramic Treatment
Treatment Menu
Bite Alignment
Treatment Menu
Wisdom Teeth
Treatment Menu
Pediatric Dentistry
Treatment Menu
Orthodontics & Clear Aligner Therapy
Treatment Menu
Check-ups & Preventive Dentistry
Treatment Menu
Root Canal Treatment
Treatment Menu
Teeth Whitening
Treatment Menu
Cosmetic Dentistry

